This morning, I had a session with my chiropractor, Dr. Maz. I walked into his recently remodeled space and took in a deep breath. There were velvety green and blue chairs, a wave-inspired rug, and an off-white paint. When I went to stretch my back on the “prep chair”, my eyes were drawn to the screen of calming waves sweeping across an unnamed beach. I sighed and stretched out each side equally.
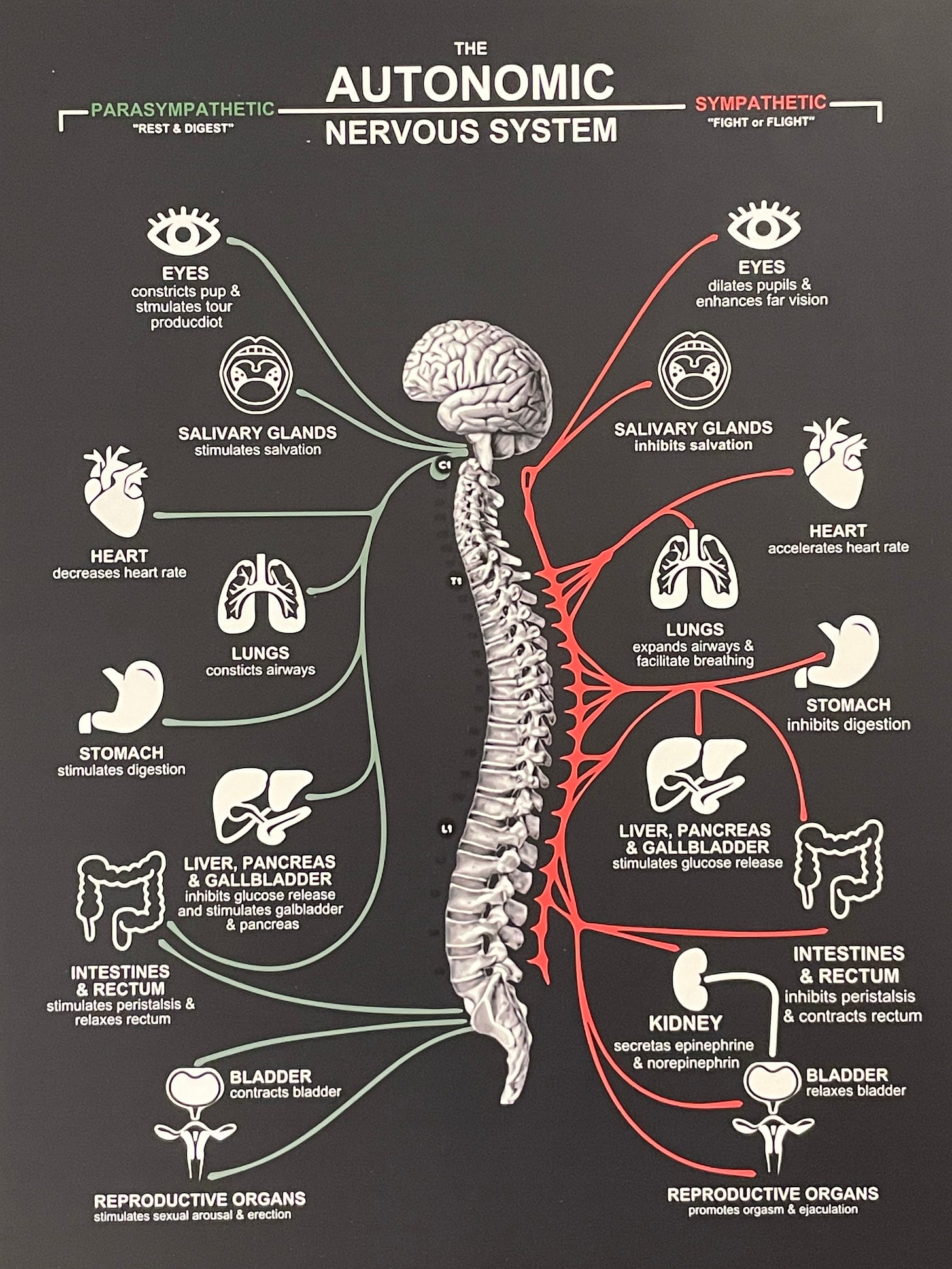
I also noticed a new sign that Dr. Maz posted of the autonomic nervous system. I smiled and snapped a photo of it, which illuminates the complexity of how interconnected the body is and how tipping the scales in one direction can affect so many organs at once.
When I got home, I had an email from a colleague who I met a couple weeks ago in Kenya. I gave a talk at Aga Khan University’s Brain & Mind Institute about my work for my forthcoming book, Invisible Illness, and I met several neuropsychologists and a translational neuroscientists, who were thinking in overlapping ways to my theoretical and narrative work but in a much more translational way (meaning, with a focus on how do we understand health and possibilities for healing). My colleague wrote to me, “I just had a patient yesterday that had at least five of the six chronic inflammatory syndromes that are part of that umbrella acronym you mentioned to me.” I nodded as I read her message—so many patients collect these cross-linked diagnoses.
One way people I’ve interviewed over the past 18 months describe these conditions is through the term “Septad.” Septad is largely a patient-driven term to explain the “alphabet soup” of diagnoses they collect. Most patients have one diagnosis placed at the center, but gather several other conditions that are perceived, at least in a clinical sense, as more peripheral. Many people are diagnosed with auto-immune conditions, such as Sjogren’s syndrome or Lupus, or connective tissue disorders like hypermobile Ehlers Danlos Syndrome. Many develop Mast Cell Activation Syndrome (MCAS) and dysautonomia or Postural Orthostatic Tachycardia Syndrome (POTS). Others have infections, such as Lyme Disease, Epstein-Barr Virus, Coxsackie B4, ME/CFS, and Long Covid. Many have gastric issues, such as gastroparesis or small intestine overgrowth. Others demonstrate structural anomalies associated with the brain and spine. “Septad” therefore refers to a Venn diagram of these often-overlapping conditions.
This is not a patient-only framework. David Kaufman, a physician working for years in HIV/AIDS research and treatment in NYC, and Ilene Ruhoy, a neurologist with expertise in environmental toxicology, co-developed the Patreon channel called Unraveled: Understanding Complex Illness last year, which discusses conditions like ME/CFS, hEDS, MCES, small figer neuropathy, POTS, infections, and environmental exposures. This is a particularly useful episode. You can also learn more from the National Institutes of Health’s ME/CFS Research Roadmap Webinar Series, “Lesser Studies Pathologies,” hosted on January 5th of this year.
Which brings me back to Dr. Maz. I had severe back pain for seven years after I had my second child. I went to a chiropractor who hurt me and swore I’d never visit one again. I tried to manage it with yoga and massage, which worked when it worked but was so painful on some days that I could barely get out of bed some mornings. My dad kept telling me that it was time to think about surgery. Before I took that route, someone recommended I try a gentle chiropractic practice—the atlas adjustment, which so gently pushes things into place. Long story short: it changed my life, even though I often regress (like after international flights!). The experience revealed to me the power of recentering the nerves and the body in quiet, gentle, repeated, and focused ways.
This morning I asked Dr. Maz if anyone with Long Covid found relief from his adjustments (and I shared the vagus nerve theory). He said, “Most likely the adjustment will realign the spine and the muscles, possibly providing relief into the nerves. I have had some Long Covid patients who said adjustments helped them deal with panic attacks.” I nodded, thinking back to how much anxiety flushed through my body after my COVID infection nearly two years ago, and how frequently anxiety and panic are described by the many Long Covid patients I’ve spoken to. This is one reason why polyvagal therapy—as one source of relief—is so frequently described as an oasis by so many patients.
I’m curious about your experiences – and where/how you found relief. Do you use the term SEPTAD and do others in your networks?